Eosinophilic esophagitis is a condition that impacts 1 in every 2,000 Americans. Many sufferers also have allergies like hayfever and asthma. Eosinophilic esophagitis (sometimes shortened to simply EoE) is caused by an immunologic reaction which presents primarily in the esophagus (not a true allergic reaction). Treatment options can vary, and so far there’s typically no “cure” for this condition. That means that most patients achieve relief by successfully managing their symptoms.
In some cases, managing symptoms will mean identifying likely triggers and avoiding them–a process that can require a specialized diet. This can be challenging for patients, but there are some tips and tricks which can help.

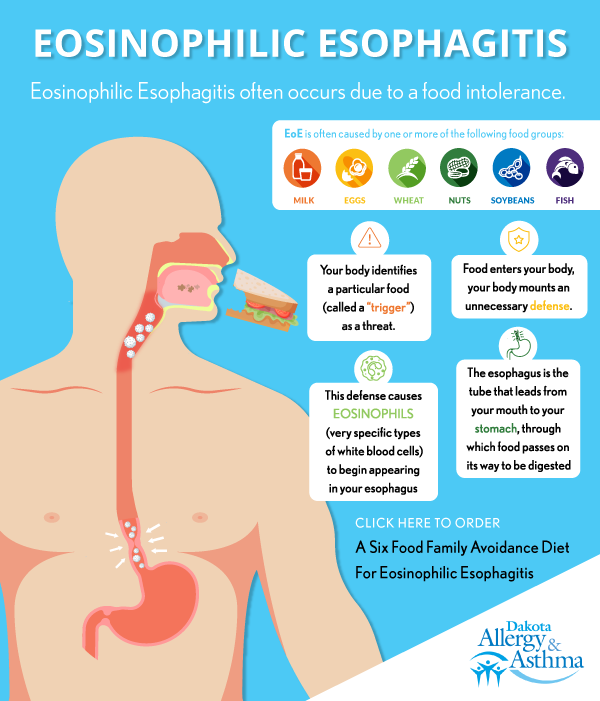
What is Eosinophilic Esophagitis?
Eosinophilic esophagitis often occurs due to a food intolerance. Your body identifies a particular food (called a “trigger” by doctors) as a threat. When this food enters your body, your body mounts an unnecessary defense. This defense causes eosinophils (very specific types of white blood cells) to begin appearing in your esophagus (the esophagus is the tube that leads from your mouth to your stomach, through which food passes on its way to be digested).
This whole response can ultimately lead to inflammation in your esophagus. And that inflammation causes some of the most noticeable presentations of EoE.
Eosinophilic Esophagitis Symptoms
For most people, eosinophilic esophagitis symptoms will include the following:
- Decreased appetite, especially in younger patients. (If eating becomes uncomfortable for kids, they’re likely to just avoid eating.)
- Difficulty eating or swallowing. It may feel as though food backs up in your esophagus as you eat.
- Regurgitation.
- Acid reflux.
- Vomiting.
- Pain in the stomach.
- Food impaction (this occurs when food gets stuck in the esophagus–if impaction does not resolve itself, it may require medical attention).
How is Eosinophilic Esophagitis Managed?
An eosinophilic esophagitis diagnosis can only come from a healthcare provider (you can’t really diagnose yourself at home) and normally involves looking at your esophagus with an endoscopy and getting biopsies of the lining. But once that diagnosis is confirmed, your Doctor may suggest a few different treatment options. They might include:
- Steroids: Sometimes, your symptoms may warrant the use of a topical steroid. In these cases, you’ll be given a prescription and detailed instructions. The idea behind steroid treatments is to help alleviate some of the inflammation in the esophagus.
- Proton Pump Inhibitor: A proton pump inhibitor is an oral medication (usually a pill) that’s designed to both decrease the inflammation and will also reduce the amount of stomach acid you produce. This can help alleviate symptoms such as acid reflux.
- Biologic Therapy: Antibodies against parts of the immune system can dramatically reduce the eosinophilic inflammation and reduce EoE symptoms. Dupixent is the first of these medications that has been shown to be effective.
- Diet therapy: Changing your diet to avoid triggers is one of the most effective ways to limit symptoms. But it’s not without challenges.
- Dilation of the esophagus: In some cases, your esophagus may become far too narrow to safely eat. In these cases, your provider may recommend a minimally invasive procedure called esophageal dilation, which uses an endoscopic balloon to stretch your esophagus.
What Does This Diet Plan Look Like?
EoE is typically caused by one or more specific foods. This isn’t a true allergy involving the allergy antibody IgE, so skin or blood allergy testing is inaccurate. Instead, a special eosinophilic esophagitis diet can help you diagnose and then manage the symptoms.
The purpose of this diet plan is to help you determine which food group is most likely to cause your symptoms so you can better avoid that group in the future. Unfortunately, your digestive system moves slowly (and, sometimes, mysteriously), making this process a somewhat lengthy one.
Typically, EoE is caused by one of the following food groups:
- Milk
- Eggs
- Wheat
- Soybeans
- Peanuts/Tree nuts
- Fish/shellfish
If you’re following an eosinophilic esophagitis diet, you’ll avoid these six groups for one to two months. At that point, you’ll be checked out by your Doctor to ensure the diet plan has successfully minimized your symptoms. This normally involves another EGD with biopsies atop of your symptoms.
After your Doctor gives you the okay, you can begin slowly reintroducing foods. You’ll want to do this one food group at a time and do each for a number of weeks. That way, if your symptoms start back up when you reintroduce soybeans, you will have successfully identified a trigger–and a food group you can avoid in the future. Repeat EGDs are a normal part of this try back period.
Work with a Dietician and Have a Menu Plan
An eosinophilic esophagitis diet can be a challenge, even with the best of intentions. The best way to succeed is to rely on a little help. You and your Doctor agree on which type of avoidance diet to go on (2 food, 4 food, or the standard 6 food family avoidance diet) and what to do with your medications while on the diet. For some patients, that might mean consulting with a dietician.
For other patients, it might mean using an already-created Six Food Family Avoidance Diet 28-day menu. Dr. Bubak has made such a menu in his book, available here.
Working with your Doctor’s Team can get you the relief you’ve been searching for!
To learn more about eosinophilic esophagitis visit the AAAAI Website or ACAAI Website, or even better—see your Doctor.




